History of Zostavax
Zostavax first came to market in the United States in 2006, and at that point, the vaccine was only approved for use in patients 60 or older. However, in 2011, the use of Zostavax was expanded to include patients between the ages of 50 and 59, meaning the vaccine was approved for patients ages 50 and older, the very age group shingles typically affects. Shingles, or the herpes-zoster virus, is the second phase of a two-part infection, the initial phase of the infection being the contraction of the varicella-zoster virus, which causes chickenpox, usually during childhood. Once the chickenpox infection runs its course and the person recovers from the disease, the varicella-zoster virus stays dormant in the body for years, or even decades. The virus can then re-emerge later in life in the form of shingles, a disease characterized by shooting pains, extreme discomfort and a full-body rash, with a band of blisters on one side of the body.
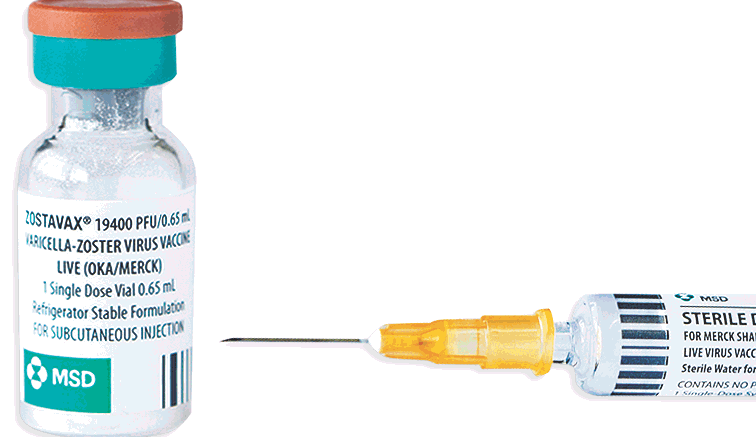
The issue with Zostavax is believed to be caused by vaccine strain virus shedding, infection and transmission, a known complication of live virus vaccines like Zostavax. When this occurs, the vaccine has the potential to cause the very disease it was designed to prevent, in this case, shingles. In some cases, instances of shingles allegedly caused by the Zostavax vaccine may progress to include treatment-resistant “post-herpetic neuralgia,” a complication of shingles causing burning nerve pain that can persist even after the initial rash has healed.
According to allegations raised in a growing number of Zostavax lawsuits, Merck & Co. discovered during premarket approval trials that the vaccine could cause patients to contract shingles, but kept this information from consumers and the medical community. It wasn’t until August 2014, years after the vaccine was approved by the FDA, that Merck added a warning to the Zostavax label highlighting the potential for the vaccine to cause shingles and other complications.